01 Jun 2019
Author: Sumithra Urs, PhD | Scientist, Scientific Development
Date: June 2019
Pancreatic cancer is the ninth most commonly diagnosed cancer and ranks as one of the deadliest with the lowest 5-year survival rate of 5-8%.[1,2,3] This year alone, the American Cancer Society estimates that 56,770 people will be diagnosed with the disease of which more than 45,750 people may not survive. Pancreatic ductal adenocarcinoma (PDAC) being the most prevalent and aggressive form of exocrine pancreatic cancer accounts for ~90% of cases with mortality equaling incidence.[4,5]
At diagnosis, a vast majority of PDAC patients have either locally advanced, unresectable, or metastatic disease. The silent spread of the disease, and appearance of disease specific symptoms only at advanced stages, makes early detection very challenging and contributes to the low survival rates. Treatment options for resectable patients include surgery followed by first line systemic chemotherapy (gemcitabine, FOLFIRINOX, paclitaxel) or combination chemoradiotherapy. For locally advanced, unresectable patients, the regimen includes multi-agent chemotherapy (5-FU, oxaliplatin, irinotecan) or chemoradiotherapy.[6] As these treatments have offered limited benefits to pancreatic cancer patients, newer options like immunotherapy drugs are now being tested in clinical trials.
PDAC are characterized by presence of fibrotic stroma, low mutational burden, lack of CD8+ T cell infiltration and presence of immunosuppressive myeloid cell populations, all of which contribute to the typical non-immunogenic tumor characteristics.[7] Current approaches to enhance treatment response focus on increasing trafficking of T cells to the tumors using agents like radiotherapy (RT). RT alone, in most solid tumors, has the potential to activate the immune system to trigger an anti-tumor immune response following cytotoxic death and release of immune stimulating signals. However, in PDAC patients, the outcome of high dose RT alone, or in combination with chemotherapy agents, remains generally unsatisfactory[8] and clinical trials with single agent immunotherapy agents indicate poor response rates as low as 1-2%.[9] At least 21 open clinical trials are currently investigating the combination of RT with other immune-stimulating agents which may be a promising avenue for PDAC treatment and merits further research.[10] Along the same line, in the preclinical platform we are evaluating single and combination therapies using the Pan02 murine PDAC model. Pan02 is a well-established Grade III adenocarcinoma model developed by chemical induction with 3-MCA (3-methylcholanthrene) in male C57BL/6 mice.[11] In this model spotlight we present in vivo data on Pan02 tumor model growth kinetics, response to immunomodulatory antibodies, focal radiation, and the combination of RT with immune modulatory agents tested in the syngeneic C57BL/6 mouse strain.
Pan02 Growth Parameters
Subcutaneous implant of Pan02 results in successful establishment of tumors that have a median doubling time of 4-5 days and mice stay on study for ~30 days post implant (Fig. 1) with no weight loss (data not shown). The growth kinetics allow for over a three-week therapeutic window to evaluate anti-tumor responses in this model.
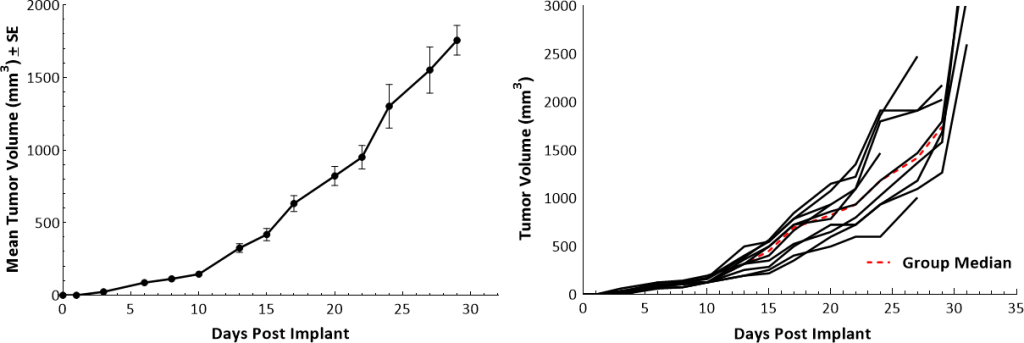
Fig. 1: Growth kinetics of subcutaneous Pan02 model in female C57BL/6 mice.
Immunophenotyping analysis of Pan02 tumors by flow cytometry confirmed the poor lymphoid cell infiltration into the tumors (Fig. 2). While CD8+ and CD4+ helper T cells constituted only 1.6% and 1% of the CD45+ population, respectively, the immunosuppressive myeloid cell populations were present in abundance. M-MDSCs and M1 and M2 TAMs were the dominant cell subpopulations. This tumor immune profile is characteristic of a non-immunogenic or “cold” tumor model, similar to what is observed in PDAC patients.
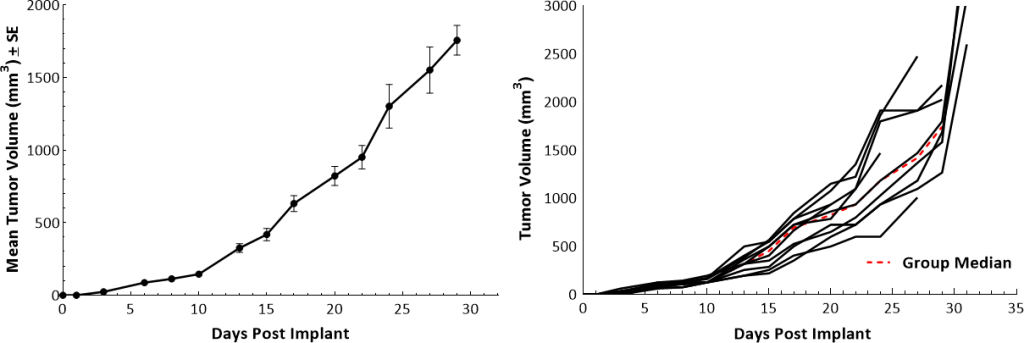
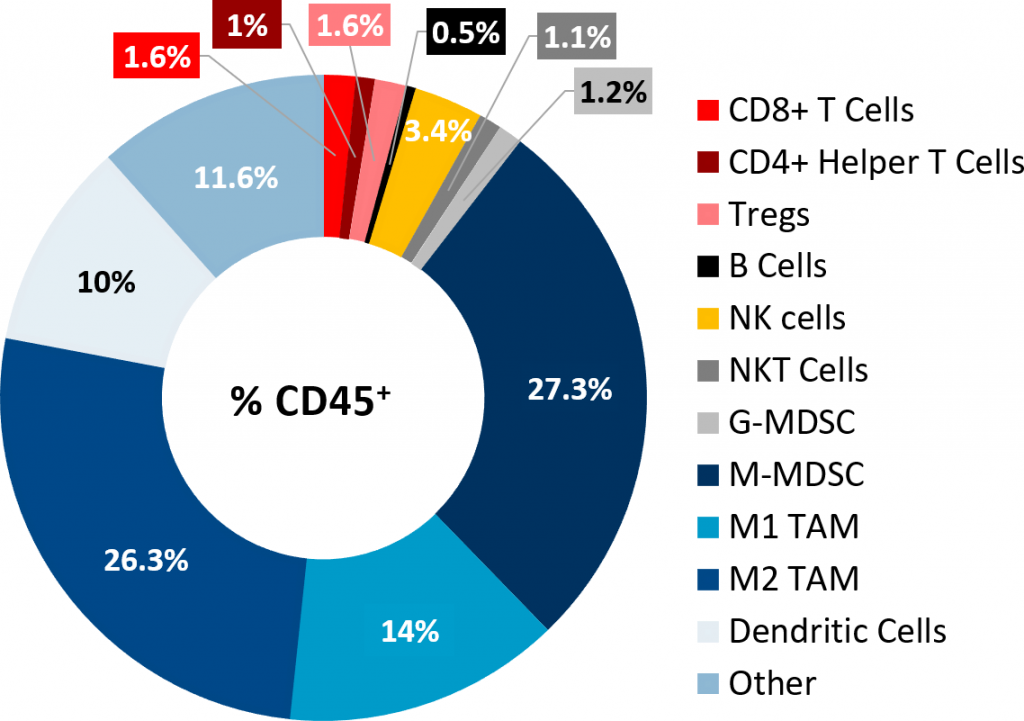
Fig. 2: Tumor immune profile of subcutaneous Pan02 tumors.
Pan02 Response to Single Agent Treatments
Single agent treatment of Pan02 tumor bearing mice with gemcitabine (100mg/kg, Q3Dx4), one of the most commonly utilized chemotherapies in pancreatic cancer patients, was well tolerated and produced statistically significant tumor growth delay (TGD) (Fig. 3).
Fig. 3: Pan02 response to Gemcitabine.
Given the investigation of immunotherapies in PDAC clinically, we set out to evaluate the responsiveness of our Pan02 model to a variety of immune-modulating antibodies (Fig. 4). However, in line with the immunosuppressive profile of the Pan02 tumors, it was not surprising that this model had minimal/no response to the checkpoint inhibitors anti-mPD-1, anti-mPD-L1 and anti-mCTLA-4, and the costimulatory antibodies anti-mCD137 and anti-mOX40. All antibodies were dosed twice weekly at 10mg/kg for a total of 4 doses (Fig. 4).
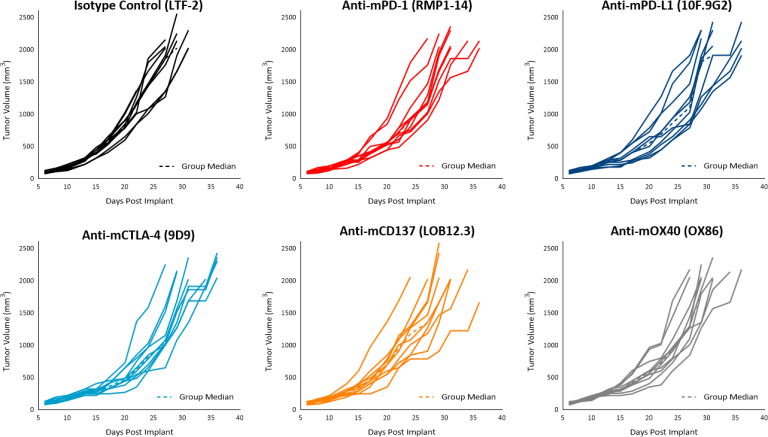
Fig. 4: Pan02 response to immune modulatory antibodies.
Pan02 Response to Radiation and Combination Treatments
Radiation therapy is commonly administered to PDAC patients. In our mouse model we employed the Small Animal Radiation Research Platform (SARRP; Xstrahl) to deliver a single dose of focal radiation (5Gy or 10Gy) directly to the tumor and we observed dose dependent tumor growth delay of 9.5 and 22 days, respectively compared to the untreated control (Fig. 5).
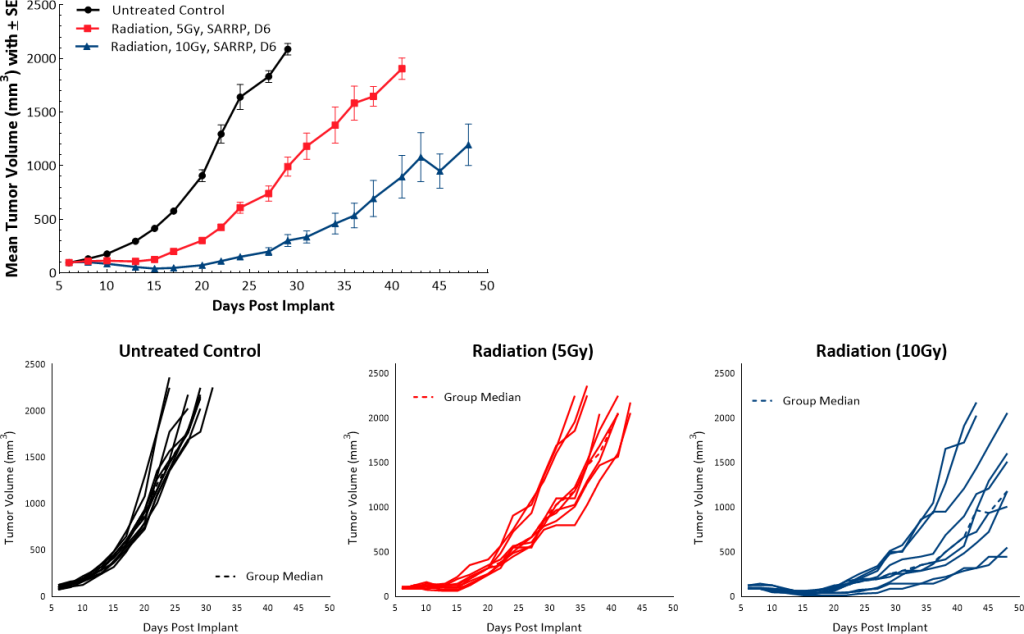
Fig. 5: Pan02 response to focal radiation.
In order to investigate the anti-tumor effects of RT in combination with checkpoint inhibitors, a single dose of 5Gy was used along with anti-mPD-1 or anti-mPD-L1 antibodies. Untreated and isotype control groups showed overlapping growth rates and treatment with single agent checkpoint inhibitors anti-mPD-1 and anti-mPD-L1 did not elicit any anti-tumor response. While a single dose of 5Gy RT resulted in a TGD of 9.5 days over the untreated control, combination with checkpoint inhibitors did not significantly contribute to improving the anti-tumor response. RT with anti-mPD-1 or with anti-PD-L1 resulted in TGD of 13 and 11.2 days, respectively (Fig. 6).
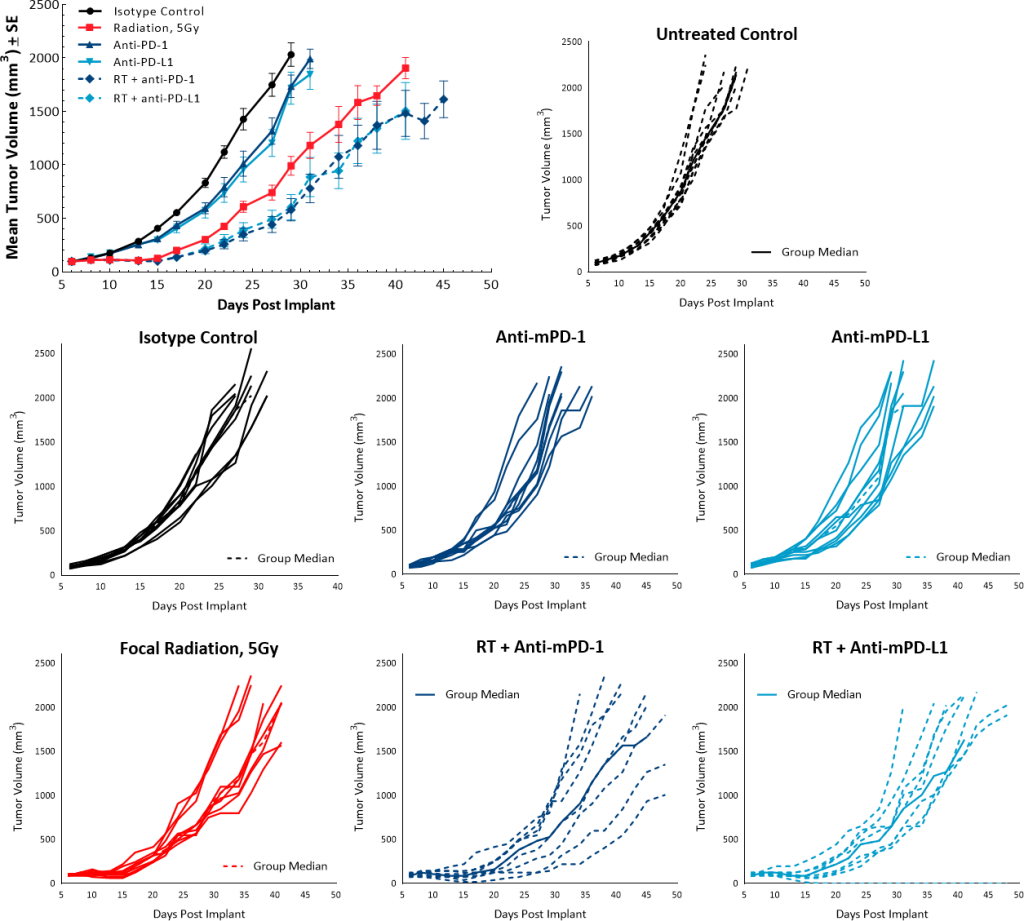
Fig. 6: Pan02 response to radiation and checkpoint inhibitor combination.
Future Work with the Pan02 Model
Studies are underway to evaluate the potential of using multiple combinations to improve treatment response in the subcutaneous Pan02 model. In addition, we have recently generated a luciferase-enabled Pan02 cell line to support studies in the orthotopic setting.
