Immune deficient mice by design lack adaptive immunity which makes them an ideal host for supporting the transplantation and growth of human tumor cells. Preclinical xenograft models utilizing immune deficient mice are limited for the investigation of immunotherapies due to this lack of functional immune cells. This spotlight will highlight a method in which human T-lymphocytes cells can propagate within an immune compromised mouse and support tumor xenograft growth.
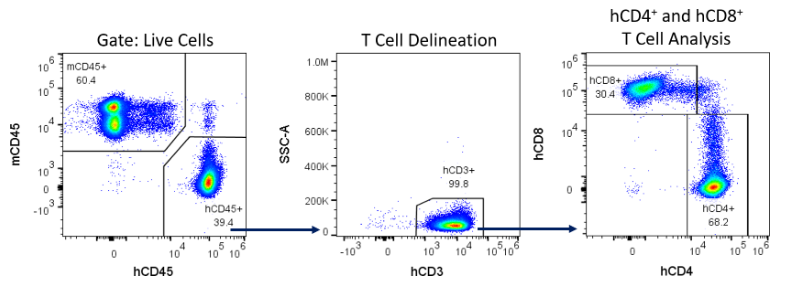
NOD-scid IL2Rγnull (NSG) mice engrafted with human peripheral blood mononuclear cells (hPBMCs) have been utilized in xenograft models with success to evaluate efficacy and pharmacodynamics of immune checkpoint inhibitors targeting epitopes on human T-Lymphocytes1. This model is unique over conventional xenografts because functional human T-cells can target human epitopes on a tumor in a mouse with directly translatable clinical significance. NSG mice are deficient in dendritic and macrophage cell populations and carry two specific mutations rendering them highly deficient of lymphocytes; the Pkrdc mutation disables aspects of DNA repair that renders the mouse B- and T-cell deficient, and deletion of IL2Rγ blocks NK cell maturation2. This combination of deficiencies allows for the engraftment of hPBMCs and allows for the expansion of human T-lymphocytes in the NSG mouse.
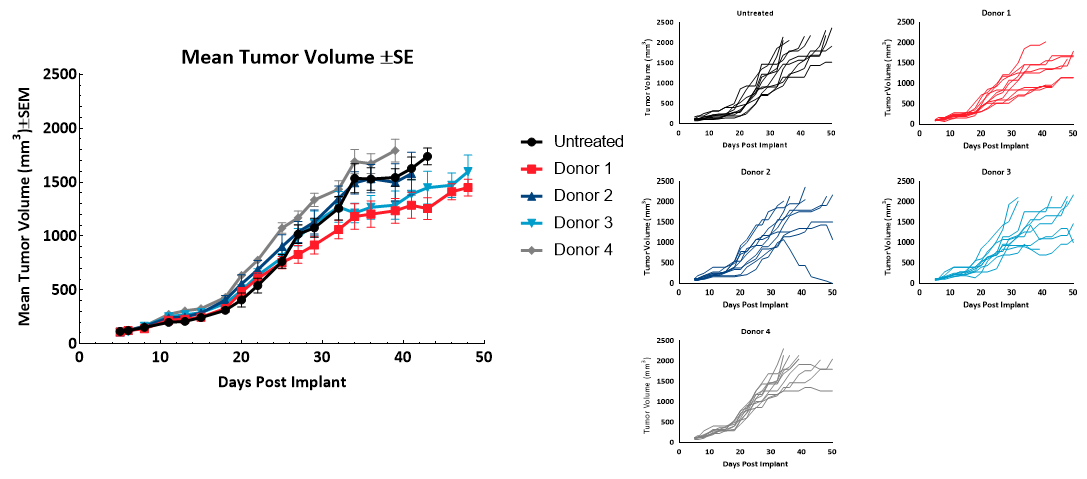
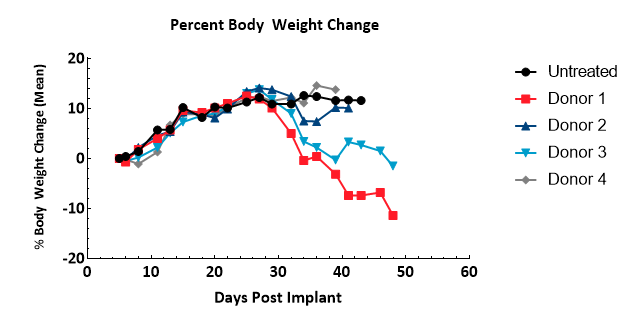
The hPBMC engrafted NSG mouse does have caveats that must be evaluated prior to human donor and tumor model selection. First, administration of human immune cells to a mouse results in T-cell mediated toxicity consistent with Graft Versus Host Disease (GvHD), in which human lymphocytes attack mouse tissues, limiting the therapeutic window3. Second, engraftment efficiency, cell types present, and activity have been observed to be variable between human donor sources4. Finally, we have observed instances of hPBMC rejection of the human tumor xenograft (data not shown). Evaluation of these parameters with the donor source and tumor model of choice, prior to initiating definitive efficacy studies, is critical for the success of translational early development programs.
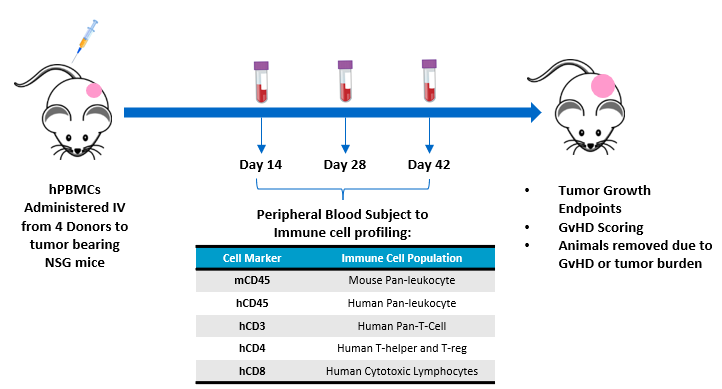
Experimental Design
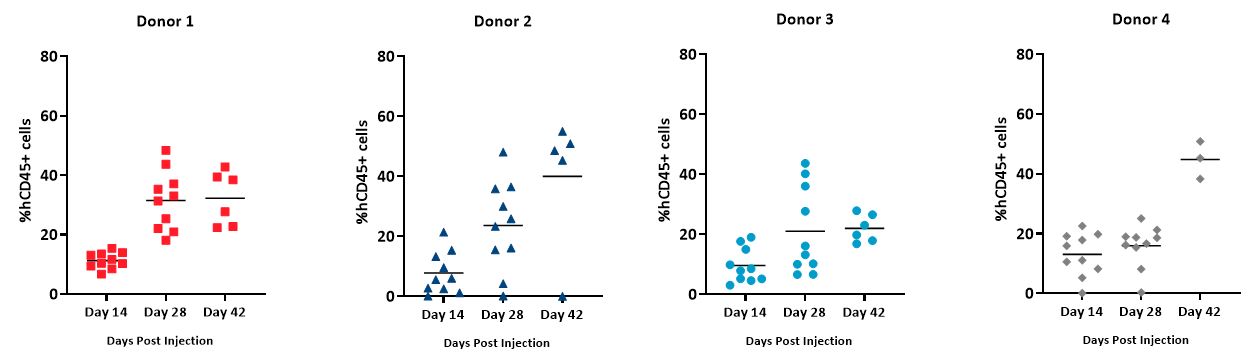
The objective of this study is to evaluate the engraftment of human T-lymphocytes from hPBMCs administered to NSG mice bearing subcutaneous human tumor xenografts. Animal care and use was performed in conformance with the Guide for the Care and Use of Laboratory Animals in an AAALAC-accredited facility. NSG mice (Jackson Laboratories, Bar Harbor Maine, USA, strain #0005557) bearing subcutaneous MiaPaCa-2 human pancreatic ductal adenocarcinomas were intravenously administered hPBMCs from four different normal healthy donors (Hemacare, Los Angeles CA, USA). Tumor growth, bodyweight and evaluation of GvHD-like characteristics were performed. Whole blood was collected for flow cytometry analysis of human lymphocyte markers to confirm donor engraftment of CD45+ cells, including CD4+ and CD8+ cells, on days 14, 28, and 42 post hPBMC administration (Figure 1).