01 Feb 2017
Author: Maryland Franklin, PhD, Vice President, Scientific Development
Date: February 2017
Glioblastoma multiforme (GBM) is the most aggressive form of brain cancer. GBM tumors grow within a fairly immunosuppressive tumor microenvironment and a relatively immune-privileged central nervous system. For patients diagnosed with GBM, prognosis remains poor with conventional therapies that include radiotherapy, chemotherapy, and surgery.
Immunotherapy drugs provide an alternate approach to treatment, aiming to bolster the immune system to eradicate disease. In the past, use of antibody therapies has been limited in GBM due to the obstruction caused by the blood brain barrier to therapy delivery. However investigation of immuno-oncology drugs may overcome this limitation as one may only need the immune cells to cross the blood brain barrier. Preclinical testing of this class of drugs requires the use of a unique set of preclinical models utilizing immunocompetent mice and orthotopic placement of the tumor cells within the brain. We have been utilizing orthotopic GBM models for more than 12 years.
GL261 is one of the most frequently used syngeneic murine glioma models available. We capitalize on our state-of-the-art imaging capabilities to further interrogate the pharmacology of this model by utilizing a GL261 cell line that expresses luciferase (GL261-luc2, Caliper Life Sciences). This allows for longitudinal, in vivo visualization of the tumor’s growth and response to treatment within the brain via bioluminescence imaging (BLI).
At Labcorp, we have acquired Xstrahl’s Small Animal Radiation Research Platform (SARRP) allowing for focal beam irradiation of the brain, sparing the rest of the mouse, including secondary lymphoid organs critical for mounting an immune response.
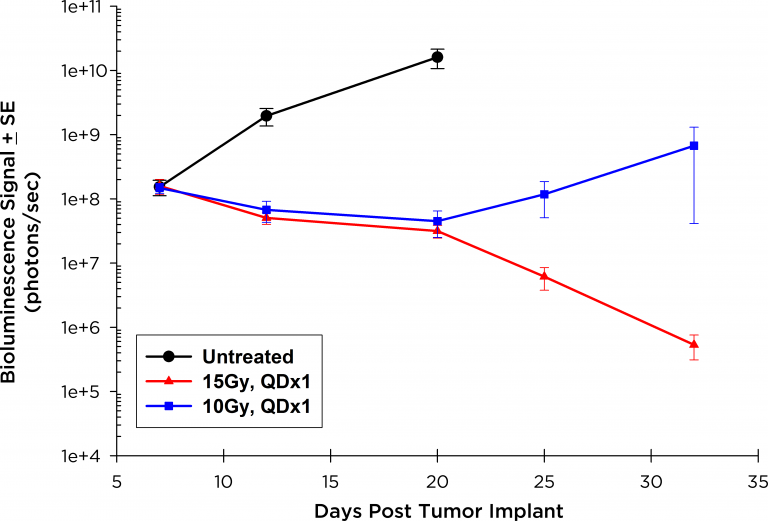
Fig. 1: Orthotopic GL261-luc: BLI Signal Over Time in the Brain
We have utilized the GL261-luc model to test focal radiation with and without the immune checkpoint inhibitor antibody, anti-PD-1. As a first step we tested two individual doses of focal irradiation to determine an optimal dose for combination studies. We observed that a single dose of 15Gy resulted in dramatic decreases in overall BLI signal (figure 1, red line) and was curative in this model (100% of mice were tumor free out to 60 days post implant). A single dose of 10Gy resulted in moderate tumor stasis followed by rapid outgrowth of tumor (figure 1, blue line) and was only moderately active with 25% survival on study day 42. Thus, in a follow on study we utilized a single dose of 10Gy with and without 10mg/kg of anti-PD-1 antibody and monitored disease progression and therapeutic benefit by BLI.
Figure 2 illustrates the BLI tracking in representative mice from each group. The group mean for each was quantified and graphically represented (figure 3). In addition, overall survival based on morbidity and mortality endpoints was calculated (figure 4). The sum of the data demonstrate some added benefit of either focal irradiation or anti-PD-1 antibody alone and improved anti-tumor activity of the two therapy combination (100% survival for more than 60 days).
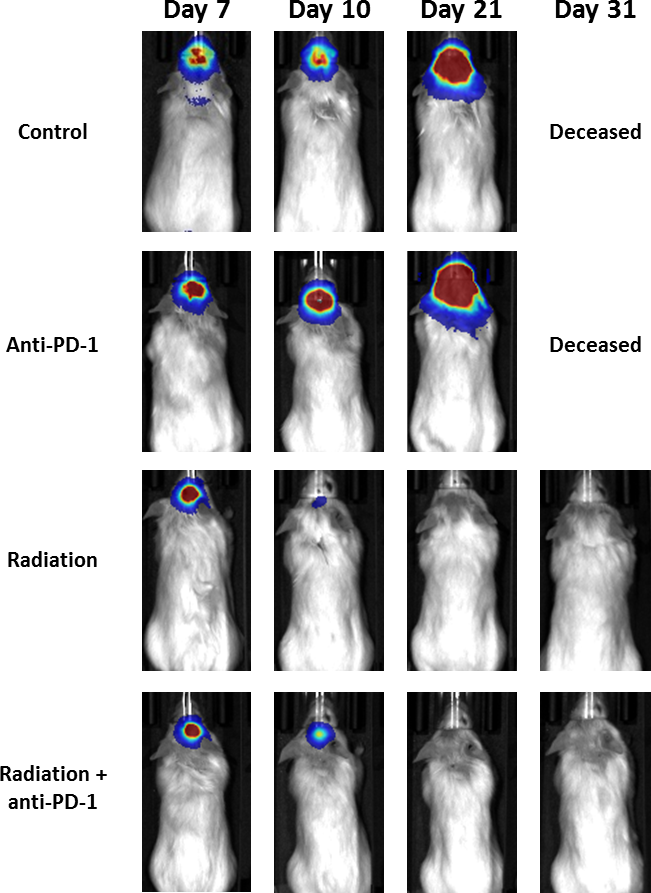
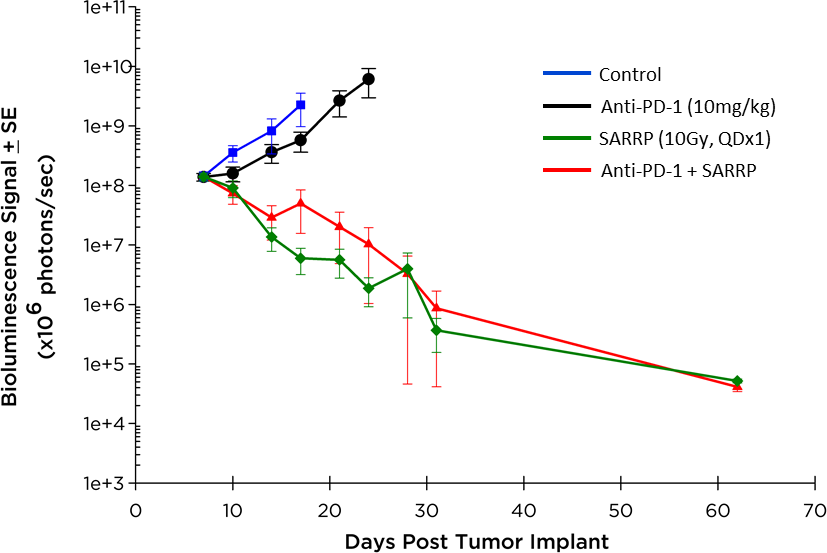
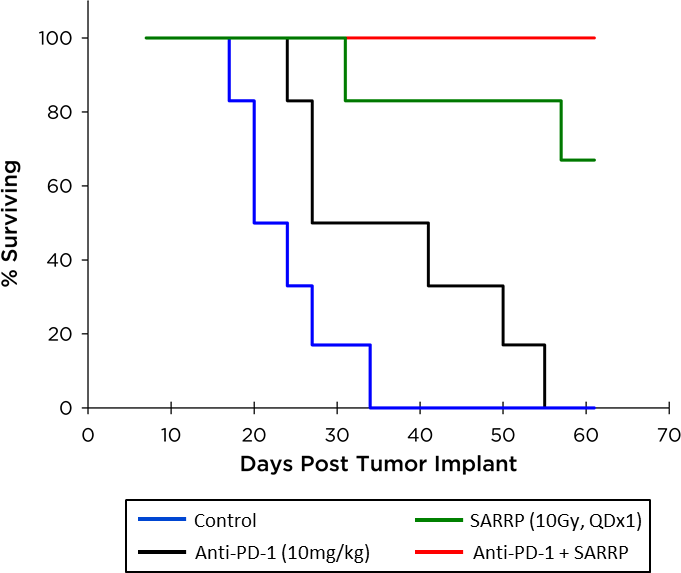
Fig. 3: Orthotopic GL261-luc: BLI Signal Over Time in the Brain
Fig. 4: Orthotopic GL261-luc: Overall Survival (Morbidity/Mortality)
In addition to bioluminescence, Labcorp has a host of other imaging technologies, including PET, SPECT, an CT modalities, to further interrogate parameters related to GBM such as tumor volume, vascular perfusion/permeability, metabolic activity, and edema. Labcorp also has comprehensive In Vitro Services including flow cytometry to best evaluate immunotherapies.
Contact us today to discuss your GL261-luc study.
