Targeted radiation: Increasing translational relevance
Radiation therapy is one of the most common treatments for cancer, which means that it is vital to understand its effect when novel cancer treatments are used. Radiation therapy uses high-energy particles or waves, such as x-rays, to destroy or damage cancer cells. However, while radiation will damage tumors, it will also harm normal tissue.
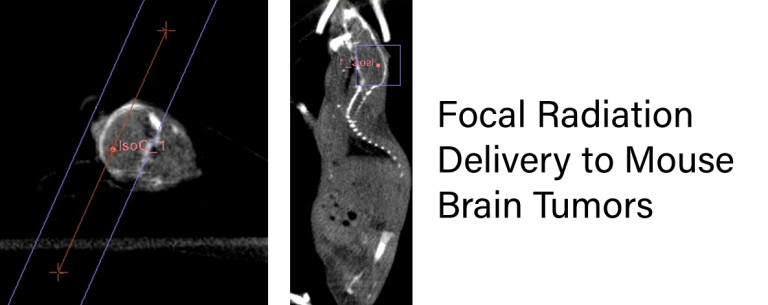
Great care is taken to spare surrounding tissue from the highest doses of radiation. By using an anatomical imaging technique such as CT, clinicians can create a treatment plan that delivers a precise therapeutic dose to the tumor alone.
We have joined with Xstrahl, a world leader in preclinical targeted x-ray irradiators, to extend this powerful technology to you as part of our service offerings. Xstrahl’s Small Animal Radiation Research Platform (SARRP) incorporates CT imaging with precise radiation delivery to enable researchers to pinpoint an exact anatomical target.
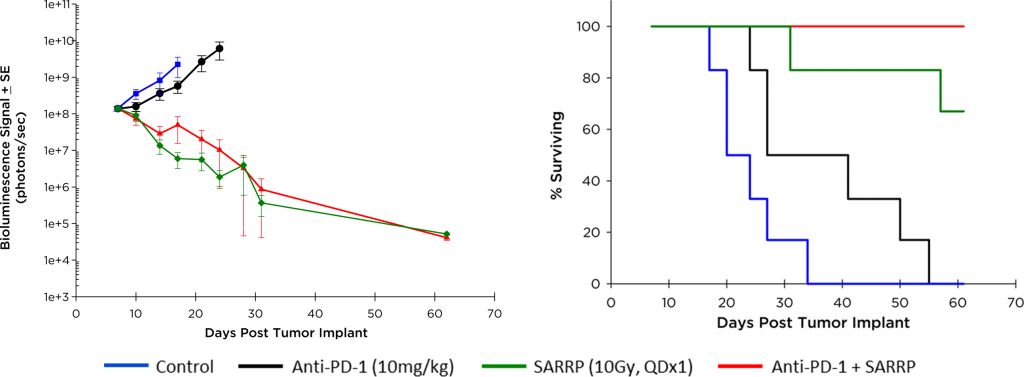
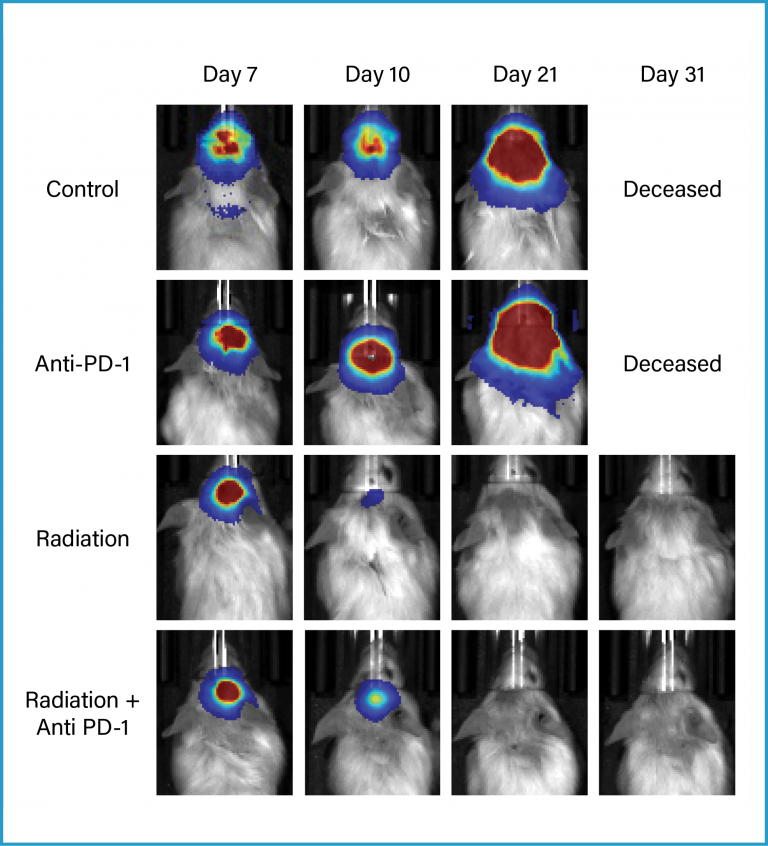
This small animal irradiator can then deliver single or multiple beams of radiation to the target with the utmost accuracy, matching the clinical techniques used in oncology departments around the world. This precision becomes important particularly in the evaluation of immune activating therapies where whole animal irradiation could inhibit and/or directly alter the animal’s innate immune system. The combination of precision radiation delivery and our expertise in immuno-oncology allows you to execute complex and powerful study designs.